What to do During a Depressive Crisis? - Severe Depressive Episode
According to national suicide-prevention guidelines, early professional help paired with social support is the single most effective way to lower suicide risk and speed recovery.
Clinical protocols recommend immediate emergency evaluation, which may involve short-term hospitalization, medication adjustments, or rapid-acting treatments when safety is at stake.
First Actions to Take when Feeling Severely Depressed
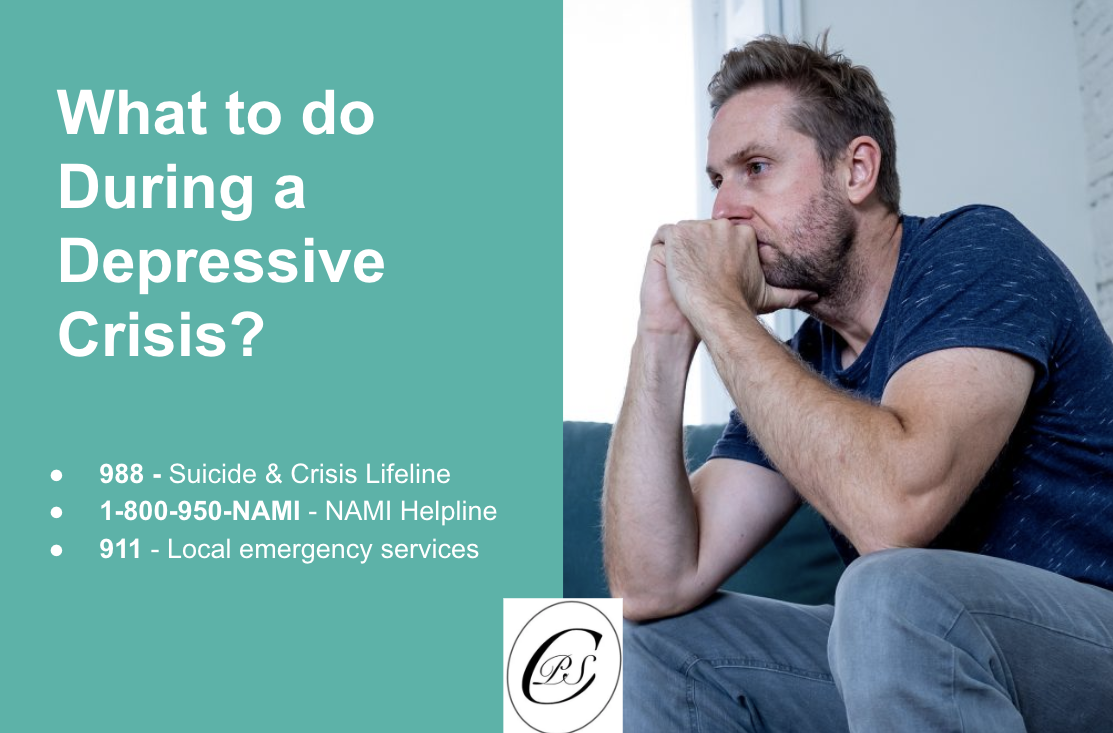
Call or text 988 (U.S.) or your country’s suicide and crisis helpline for 24/7, free support from trained counselors.
If you feel unsafe or cannot stay alive, call 911 or go to the nearest emergency department. Emergency assessment is strongly recommended when suicidal intent is present.
Contact your psychiatrist or therapist for urgent medication review or a same-day visit.
Reach out to a trusted friend or family member. Research shows that immediate social support significantly lowers acute suicide risk.
Remove or avoid access to harmful items such as weapons, medications, or sharp objects—clinical reviews emphasize means-restriction as a key protective step.
Key Resources for Seeking Help with a Depressive Episode
988 Suicide & Crisis Lifeline (U.S.) – Call or text 988 anytime.
NAMI Helpline – 1-800-950-NAMI for mental health information and support.
Local emergency services – Dial 911 in the U.S. or your country’s equivalent for immediate danger.
International helplines for crisis numbers outside the U.S.
Understanding a Depressive Crisis — What Counts as a Crisis?
A depressive crisis is a rapid, severe worsening of symptoms that makes daily life unsafe or impossible — for example, sudden deep sadness, loss of interest, or extreme fatigue that prevents basic functioning. According to major clinical reviews, these core symptoms (low mood, anhedonia, exhaustion) are central to crisis states.
When a crisis includes suicidal thoughts or self-harm urges, the risk is immediate and demands urgent intervention — hopelessness and past attempts are among the strongest predictors of acute suicide risk. According to meta-analyses, escalating suicidal ideation is a red flag.
Acute impairment in functioning — not being able to get out of bed, care for yourself, or communicate — is itself a crisis marker. Clinical guides treat severe functional decline as grounds for emergency assessment.
Why does a Depressive Crisis Happen?
Crises often arise when multiple stressors align: a major life event, abrupt treatment change, or stopping medication can tip someone from stable into crisis. Network and clinical studies show negative events commonly trigger rapid symptom escalation.
Biological drivers also matter: sleep disruption, stress-hormone (HPA) activation, neurotransmitter, and reward-circuit dysfunction can amplify symptoms quickly. Recent mechanistic reviews link these biological changes to sudden worsening.
Psychological and social factors — isolation, maladaptive coping (e.g., substance use), and weak support systems — further increase the chance that symptoms will spiral into a crisis. According to network analyses, social support is a key protective factor.
Recognizing Warning Signs of a Depressive Episode Early
Watch for swift changes in mood, energy, or sleep — worsening anhedonia, severe insomnia or hypersomnia, and marked fatigue are common early signals of decompensation. Longitudinal studies show these symptoms predict escalation.
Pay attention to feelings of being trapped, disconnected, or like a burden — these cognitive shifts often precede suicidal thinking and are important warning signs to act on early. Relationship and emotion-regulation research highlights this pattern.
If you notice escalating thoughts of self-harm or suicide, treat that as an emergency. Evidence reviews identify escalation of suicidal ideation as the most actionable predictor of imminent risk.
Professional Help and Follow-Up
Contacting Your Psychiatrist: According to major depressive disorder treatment guidelines, urgent visits allow for rapid medication adjustments, bridging prescriptions, or hospital admission if needed.
Therapy Support: Crisis counseling and cognitive-behavioral interventions help contain suicidal thoughts and provide coping tools. Randomized trials confirm that brief CBT sessions reduce short-term suicide risk.
Medication Review: Missed doses or sudden discontinuation can trigger withdrawal or rebound symptoms. Clinical reviews recommend supervised tapering or reinstatement to stabilize brain chemistry.
Creating a Personal Crisis Plan
A written crisis plan helps you act quickly if warning signs return. List your early warning symptoms (e.g., worsening insomnia, hopelessness, self-harm thoughts). Include emergency contacts—psychiatrist, therapist, crisis hotlines, and safe places such as hospitals or friends’ homes.
Identify coping strategies that work for you: breathing exercises, supportive people, or grounding techniques. Evidence shows that personalized safety plans significantly lower repeat suicide attempts.
Ongoing Prevention
Prevention starts with regular therapy or psychiatry appointments to track mood changes and adjust treatment before a crisis develops. Maintain medication adherence and regular monitoring to avoid withdrawal or symptom rebound. Build healthy routines—consistent sleep, balanced nutrition, physical activity—which meta-analyses show reduce relapse rates. Join support groups or peer networks; according to longitudinal studies, ongoing social connection is protective against recurrent depressive episodes.
If you are struggling with depression or worry about a possible crisis, our team at Psychiatric Specialty Center in Wellington, FL can help you create a personalized plan and provide treatment options to keep you safe. Contact us today to schedule an appointment.