What to do During a Depressive Crisis? - Severe Depressive Episode
According to national suicide-prevention guidelines, early professional help paired with social support is the single most effective way to lower suicide risk and speed recovery.
Clinical protocols recommend immediate emergency evaluation, which may involve short-term hospitalization, medication adjustments, or rapid-acting treatments when safety is at stake.
First Actions to Take when Feeling Severely Depressed
Call or text 988 (U.S.) or your country’s suicide and crisis helpline for 24/7, free support from trained counselors.
If you feel unsafe or cannot stay alive, call 911 or go to the nearest emergency department. Emergency assessment is strongly recommended when suicidal intent is present.
Contact your psychiatrist or therapist for urgent medication review or a same-day visit.
Reach out to a trusted friend or family member. Research shows that immediate social support significantly lowers acute suicide risk.
Remove or avoid access to harmful items such as weapons, medications, or sharp objects—clinical reviews emphasize means-restriction as a key protective step.
Key Resources for Seeking Help with a Depressive Episode
988 Suicide & Crisis Lifeline (U.S.) – Call or text 988 anytime.
NAMI Helpline – 1-800-950-NAMI for mental health information and support.
Local emergency services – Dial 911 in the U.S. or your country’s equivalent for immediate danger.
International helplines for crisis numbers outside the U.S.
Understanding a Depressive Crisis — What Counts as a Crisis?
A depressive crisis is a rapid, severe worsening of symptoms that makes daily life unsafe or impossible — for example, sudden deep sadness, loss of interest, or extreme fatigue that prevents basic functioning. According to major clinical reviews, these core symptoms (low mood, anhedonia, exhaustion) are central to crisis states.
When a crisis includes suicidal thoughts or self-harm urges, the risk is immediate and demands urgent intervention — hopelessness and past attempts are among the strongest predictors of acute suicide risk. According to meta-analyses, escalating suicidal ideation is a red flag.
Acute impairment in functioning — not being able to get out of bed, care for yourself, or communicate — is itself a crisis marker. Clinical guides treat severe functional decline as grounds for emergency assessment.
Why does a Depressive Crisis Happen?
Crises often arise when multiple stressors align: a major life event, abrupt treatment change, or stopping medication can tip someone from stable into crisis. Network and clinical studies show negative events commonly trigger rapid symptom escalation.
Biological drivers also matter: sleep disruption, stress-hormone (HPA) activation, neurotransmitter, and reward-circuit dysfunction can amplify symptoms quickly. Recent mechanistic reviews link these biological changes to sudden worsening.
Psychological and social factors — isolation, maladaptive coping (e.g., substance use), and weak support systems — further increase the chance that symptoms will spiral into a crisis. According to network analyses, social support is a key protective factor.
Recognizing Warning Signs of a Depressive Episode Early
Watch for swift changes in mood, energy, or sleep — worsening anhedonia, severe insomnia or hypersomnia, and marked fatigue are common early signals of decompensation. Longitudinal studies show these symptoms predict escalation.
Pay attention to feelings of being trapped, disconnected, or like a burden — these cognitive shifts often precede suicidal thinking and are important warning signs to act on early. Relationship and emotion-regulation research highlights this pattern.
If you notice escalating thoughts of self-harm or suicide, treat that as an emergency. Evidence reviews identify escalation of suicidal ideation as the most actionable predictor of imminent risk.
Professional Help and Follow-Up
Contacting Your Psychiatrist: According to major depressive disorder treatment guidelines, urgent visits allow for rapid medication adjustments, bridging prescriptions, or hospital admission if needed.
Therapy Support: Crisis counseling and cognitive-behavioral interventions help contain suicidal thoughts and provide coping tools. Randomized trials confirm that brief CBT sessions reduce short-term suicide risk.
Medication Review: Missed doses or sudden discontinuation can trigger withdrawal or rebound symptoms. Clinical reviews recommend supervised tapering or reinstatement to stabilize brain chemistry.
Creating a Personal Crisis Plan
A written crisis plan helps you act quickly if warning signs return. List your early warning symptoms (e.g., worsening insomnia, hopelessness, self-harm thoughts). Include emergency contacts—psychiatrist, therapist, crisis hotlines, and safe places such as hospitals or friends’ homes.
Identify coping strategies that work for you: breathing exercises, supportive people, or grounding techniques. Evidence shows that personalized safety plans significantly lower repeat suicide attempts.
Ongoing Prevention
Prevention starts with regular therapy or psychiatry appointments to track mood changes and adjust treatment before a crisis develops. Maintain medication adherence and regular monitoring to avoid withdrawal or symptom rebound. Build healthy routines—consistent sleep, balanced nutrition, physical activity—which meta-analyses show reduce relapse rates. Join support groups or peer networks; according to longitudinal studies, ongoing social connection is protective against recurrent depressive episodes.
If you are struggling with depression or worry about a possible crisis, our team at Psychiatric Specialty Center in Wellington, FL can help you create a personalized plan and provide treatment options to keep you safe. Contact us today to schedule an appointment.
How Do We Decide which Depression Treatment is Right For You? Our 7-step Diagnosis Process
One of the most common concerns patients share when starting treatment is, “How do you know which treatment is best for my situation?”
At Psychiatric Specialty Center in Wellington, FL, our psychiatrists and therapists use a personalized approach based on clinical science, patient history, and your unique needs. According to recent research, treatment decisions for depression rely on a combination of clinical, personal, and contextual factors—not a one-size-fits-all formula.
Step 1: Comprehensive Evaluation Comes First
The process begins with a thorough psychiatric evaluation. Your psychiatrist reviews your symptoms, medical history, and mental health background to understand how depression is affecting your daily life. According to clinical guidelines, the severity and type of symptoms—such as the presence of suicidality or significant anxiety—are key to determining whether medication, therapy, or a combination is recommended.
Step 2: Reviewing Your Treatment History and Past Responses
If you have tried treatment before, your previous responses and side effects guide next steps. For example, if a certain antidepressant caused intolerable side effects or failed to improve symptoms, your psychiatrist may recommend a different medication or add psychotherapy to enhance results.
Step 3: Assessing Current Symptoms and Severity
Your current symptom intensity and patterns play a major role in treatment choice. Mild depression may respond well to psychotherapy alone, while moderate to severe depression often benefits from a combination of therapy and medication.
Step 4: Considering Medical Factors and Safety
Biological and medical factors are carefully evaluated. Age, cognitive function, and co-existing medical conditions can influence which treatment is safest and most effective. For example, studies show that cognitive impairment in older adults can predict how well certain antidepressants will work.
Step 5: Aligning With Your Lifestyle and Personal Preferences
Your preferences matter—a lot. According to research, patients who receive their preferred treatment (therapy, medication, or both) have better outcomes and are more likely to stick with their plan. Whether you prefer natural approaches, talk therapy, or medication, these preferences are integrated into the decision-making process.
Step 6: Evidence-Based Recommendations for Your Unique Case
Psychiatrists follow evidence-based guidelines but also use clinical judgment to tailor care. While treatment algorithms exist, doctors often incorporate patient narratives, risk factors, and nuanced clinical observations to create an individualized plan.
Step 7: Collaborative Decision-Making With You at the Center
The final decision is collaborative. Your psychiatrist will explain all recommended options, discuss potential benefits and side effects, and answer your questions. This partnership ensures the chosen treatment is both effective and acceptable to you.
Personalized Care Is the Best Care
Choosing the right treatment for depression isn’t about finding a single “best” option—it’s about finding the best fit for you. At Psychiatric Specialty Center, we combine science, experience, and your preferences to create a plan that promotes real, lasting improvement.
If you’re wondering which treatment option is right for you, schedule a consultation with our Wellington team today. We’ll help you understand your options and design a plan that fits your needs, lifestyle, and goals.
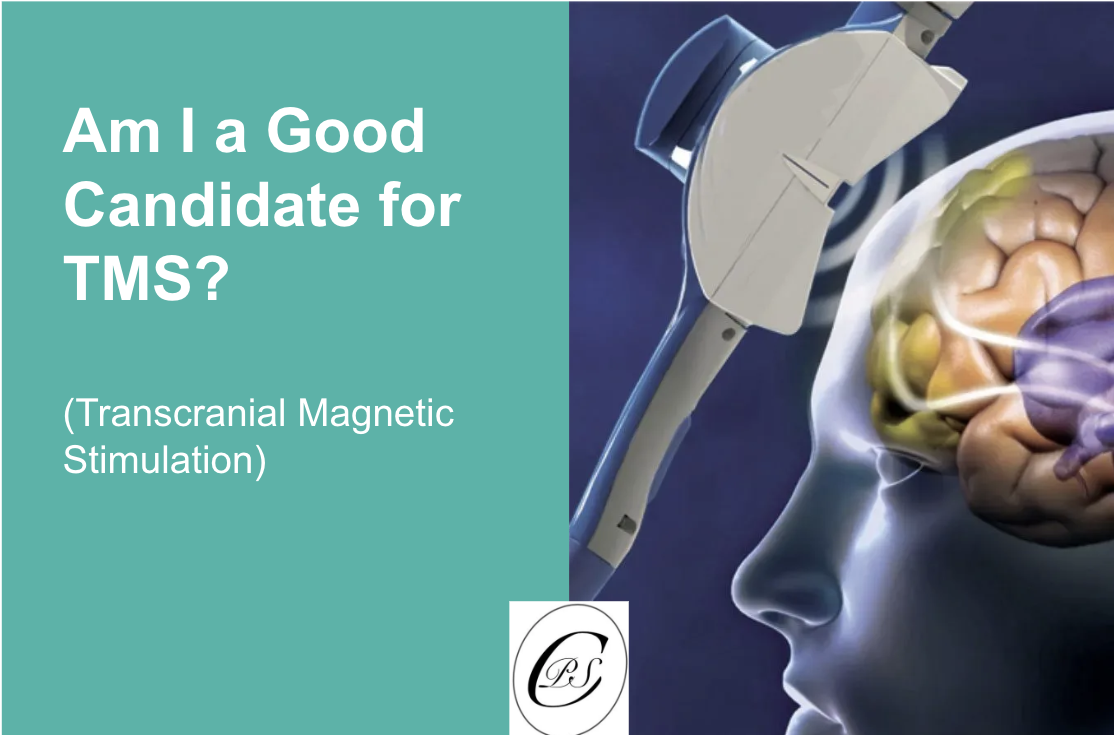
Am I a Good Candidate for TMS?
Transcranial Magnetic Stimulation (TMS) has emerged as a promising treatment for people with depression who have not improved with traditional therapies. But how do you know if you are a good candidate for TMS? According to recent clinical evidence and psychiatric guidelines, the answer depends on your treatment history, symptom severity, and medical profile. Let’s explore what research shows and what to discuss with your mental health provider before considering TMS.
Key Criteria for TMS Candidacy
1. Treatment-Resistant Depression
The strongest indicator for TMS is a history of depression that has not improved after trying at least one antidepressant medication. In many cases, providers prefer that patients have attempted two or more medications before considering TMS. If you’ve tried antidepressants without success or cannot tolerate their side effects, TMS may be a suitable next step.
2. Moderate to Severe Symptoms
Candidates typically have moderate to severe depression, especially when symptoms interfere with daily life, work, or relationships. If your depression significantly limits your ability to function, TMS may help restore balance without the systemic side effects of medication.
3. Intolerance to Medications
Some patients are unable to take antidepressants because of side effects like weight gain, sexual dysfunction, or sleep disturbances. According to clinical guidelines, TMS may be considered when medication side effects make standard treatments impractical.
4. Special Populations
Research also explores TMS for other conditions such as anxiety, OCD, and certain types of chronic pain.
Who Should Not Receive TMS?
While TMS is safe and well-tolerated for most people, there are important contraindications. According to clinical safety guidelines, individuals with a history of seizures, certain types of brain injury, or metal implants in or near the head (with the exception of dental fillings) should not undergo TMS. People with implanted medical devices like pacemakers also require careful evaluation before treatment. A thorough screening by a trained psychiatrist is essential to rule out these risks.
What to Expect from a TMS Evaluation?
Before starting TMS, you’ll undergo a comprehensive assessment that includes:
A review of your treatment history to confirm adequate trials of antidepressants.
A symptom severity assessment, which may use standardized tools like the PHQ-9 or Hamilton Depression Rating Scale.
A medical screening to check for contraindications such as metal implants or seizure disorders.
This evaluation ensures that TMS is both safe and likely to be effective for your individual situation.
Next Steps: Discussing TMS With a Specialist
According to clinical studies, TMS can provide significant relief for adults with depression who have not responded to standard treatments. However, deciding whether TMS is right for you requires a personalized assessment from a mental health professional.
If you’re experiencing moderate to severe depression, struggling with medication side effects, or wondering whether you meet the criteria for TMS, our team at Psychiatric Specialty Center can help. We provide thorough evaluations to determine if TMS—or another treatment—fits your needs.
What Is TMS and Why IS it Used for Depression?
TMS is a non-invasive brain stimulation treatment that uses magnetic pulses to target specific areas of the brain involved in mood regulation. According to clinical data, it is primarily recommended for adults with major depressive disorder who have not responded to at least one antidepressant at an adequate dose and duration. This makes TMS one of the most important options for individuals with treatment-resistant depression—a condition where standard medications have not brought sufficient relief.
What if I Want to Stop Taking my Antidepressant Medication?
Many people reach a point in treatment where they wonder if it’s time to stop their medication. Some feel better and think they no longer need it. Others struggle with side effects or simply don’t like relying on a daily pill. According to a 2020 British Journal of Clinical Pharmacology review, patients often cite side effects, cost, or feeling “well enough” as reasons for wanting to stop. This is a common and valid question—but stopping requires careful planning to avoid serious risks.
Do I need to take depression medications forever?
The short answer is no, most people do not need to take antidepressants forever. But stopping should be a medical decision, not a solo experiment. According to a 2021 Cochrane review, abrupt discontinuation raises the risk of relapse and adverse effects compared to a guided taper. Your psychiatrist can help determine whether you’ve reached a stable point where tapering makes sense, considering your history of depression, number of episodes, and current symptom control.
Common Reasons Patients Want to Stop
Patients commonly stop or reduce antidepressants because of side effects, weight changes, emotional blunting, or the feeling of being “dependent” on medication. According to a 2023 longitudinal study in Primary Health Care Research & Development, financial strain and frustration with slow results are frequent triggers. Some simply feel ready after months of remission. Whatever the reason, it’s essential to separate life changes (like improved mood) from medication effects, because feeling better can also signal that the medicine is working.
The Right Way to Reduce or Stop: Communication and Tapering
Stopping safely almost always means gradual tapering under medical supervision. According to a 2023 systematic review, reducing the dose in small steps over weeks or months lowers the risk of withdrawal symptoms and relapse. Hyperbolic tapering—reducing by progressively smaller amounts—may be necessary for some patients who are sensitive to dose changes. Regular check-ins with your psychiatrist help track symptoms and adjust the tapering schedule if problems arise.
The Hidden Risks of Stopping Suddenly
Stopping “cold turkey” can trigger intense withdrawal symptoms, sometimes mistaken for a relapse of depression. Studies report anxiety, insomnia, mood swings, dizziness, and flu-like symptoms that can last weeks or months. According to The New England Journal of Medicine, abrupt discontinuation significantly increases relapse rates within the first year compared to continued therapy. That’s why sudden self-directed discontinuation is strongly discouraged.
How Depression Medicines Work—and Why Patience Is Important
Antidepressants slowly alter brain chemistry by increasing the availability of neurotransmitters like serotonin. Because these changes take time, both starting and stopping require patience. According to a 2022 review in Therapeutic Advances in Psychopharmacology, the brain needs weeks or months to readjust after dose changes. Gradual tapering gives your nervous system time to recalibrate and reduces withdrawal severity.
Exploring Other Treatment Options With Your Psychiatrist
If you’re considering stopping medication, ask about alternatives. Cognitive behavioral therapy, mindfulness-based cognitive therapy, and lifestyle changes can help maintain remission. According to The Annals of Family Medicine, therapy during tapering improves success rates and lowers relapse risk. For some, treatments like Transcranial Magnetic Stimulation (TMS) may also be an option when medications are no longer desired or tolerated.
Importance of Communication
Perhaps the most critical step is talking to your doctor. According to a 2019 Journal of Affective Disorders review, lack of guidance and clinician support is one of the biggest barriers to safe discontinuation. Open communication allows for a personalized taper plan, psychological support, and monitoring for early signs of relapse.
How long do I need to take depression medication for?
The length of time you may need to stay on antidepressant medication depends on your unique situation, but most clinical evidence points to a minimum continuation period of 6–9 months after symptoms have improved.
For individuals with recurrent or chronic depression, or those at higher relapse risk, longer treatment—up to two years or more—is frequently advised.
According to a 2024 meta-analysis by Hu et al., stopping antidepressants too soon—especially before the three-month mark—carries a significantly higher risk of relapse compared to staying on treatment for at least three months after remission. Similarly, a landmark fluoxetine trial found that people who continued therapy for an additional 26 weeks after their symptoms lifted had a markedly lower relapse rate than those who stopped earlier.
Guidelines generally recommend continuing for at least six months after full symptom resolution, and often up to nine months, to help the brain stabilize and reduce the chance of depressive symptoms returning.
Do I Have to Stay on Antidepressants Forever?
Medication as a bridge, not a lifelong crutch
No—most people do not need to remain on antidepressants for life. For many, antidepressants are intended as a temporary bridge to stabilize mood while therapy, lifestyle changes, or other supports take hold. While some people with chronic or recurrent depression may benefit from multi-year or even indefinite maintenance, the majority can eventually transition off medication once they’ve had sustained remission and a clear plan for support.
When it comes time to stop medication, slow tapering is critical. Horowitz et al. demonstrated that gradually lowering the dose in a hyperbolic pattern over weeks to months reduces withdrawal symptoms and supports a smoother transition off treatment. Any decision to taper or discontinue should always be made with a healthcare provider, as individual factors such as age, treatment response, and number of past episodes play a major role in determining the safest plan
How Soon Will I Feel Better After Starting Depression Medication?
One of the first questions people ask after starting an antidepressant is, “When will I start to feel like myself again?” The answer depends on the type of medication and your unique biology—but here’s what research and clinical experience show:
Typical Timeline With Standard Antidepressants
Early relief (1–2 weeks): Many patients notice small but encouraging changes—like better sleep, more energy, or a slight lift in mood—within the first couple of weeks of taking an SSRI or SNRI.
Full effect (4–6 weeks): For most people, the major improvements—less sadness, more motivation, clearer thinking—take about a month to six weeks of consistent daily dosing.
Early response matters: Studies show that if you feel at least a little better within the first two weeks, you’re more likely to experience strong benefits by week six. If nothing changes by then, your prescriber may discuss adjusting the dose or switching medications.
Patient matters when taking medication to manage depression. Antidepressants don’t work like a pain pill. They slowly rebalance brain chemistry and nerve connections.
What medications are used to resolve depression? And how do they work?
The most common starting point is a group of medicines called SSRIs, or selective serotonin reuptake inhibitors. They increase serotonin, a chemical messenger linked to mood regulation, by preventing the brain from reabsorbing it too quickly. Popular options in this class include fluoxetine (Prozac), sertraline (Zoloft), and citalopram (Celexa). SSRIs are often chosen first because they’re effective, generally well tolerated, and available as inexpensive generics.
Another widely used group is SNRIs, which stands for serotonin–norepinephrine reuptake inhibitors. These medications, such as venlafaxine (Effexor) and duloxetine (Cymbalta), work on both serotonin and norepinephrine, which can help lift mood while also boosting energy and motivation.
If these first-line options don’t provide enough relief, doctors may consider atypical antidepressants. These medicines act on different brain chemicals like dopamine or a combination of pathways. Bupropion (Wellbutrin), for example, tends to be energizing and is less likely to cause sexual side effects, while mirtazapine (Remeron) can promote sleep and appetite, making it helpful when insomnia or weight loss is an issue.
Older classes such as tricyclic antidepressants and MAOIs are still available and sometimes used when newer medications haven’t worked. They can be very effective but often come with more side effects or dietary restrictions, so they require closer monitoring.
For people with treatment-resistant depression, a newer option is ketamine or its FDA-approved nasal spray form, esketamine (Spravato). These treatments target NMDA receptors in the brain and can relieve symptoms within hours or days, rather than weeks, though they’re generally reserved for cases where other medications haven’t helped.
At Psychiatric Specialist Center in Wellington, FL, we do NOT prescribe Benzodiazepines (Xanax, Klonopin, Ativan, Valium) except for RARE exceptions. These medications will not be prescribed for new patients. These medications will not be prescribed at all if you are also taking an opioid or Ambien.
Typical Costs of Antidepressant Medication
Generic SSRIs and SNRIs are often surprisingly affordable, sometimes as little as $4 to $15 a month with insurance or discount programs. Atypical antidepressants and brand-name versions may range from $20 to $100 monthly, depending on coverage. Ketamine and esketamine treatments are more costly, usually running several hundred dollars per session, and insurance coverage can vary widely.
Common Side Effects
All medications carry some risk of side effects, but most are manageable and often improve after the first few weeks. SSRIs and SNRIs can cause nausea, sleep changes, or sexual side effects. Bupropion may increase energy but sometimes leads to insomnia, while mirtazapine may cause drowsiness or weight gain. Tricyclics and MAOIs can lead to dry mouth, constipation, or blood-pressure changes and require careful supervision. Ketamine treatments are given in a clinical setting and can cause temporary dizziness or a brief sense of disconnection from reality during the session.
Who Is a Good Candidate for Medication?
Medication is usually considered when:
Depression is moderate to severe. If symptoms are significantly affecting your work, relationships, or daily life, antidepressants are often recommended—either alone or combined with therapy.
Therapy alone isn’t enough. If counseling or lifestyle changes haven’t provided enough relief after a reasonable trial, adding medication can help.
There’s a history of relapse. People who’ve had repeated depressive episodes may benefit from medication to reduce future risk.
Personal factors support it. Your previous response to treatment, side-effect profile, other medical conditions, and personal preference all play a role.
For mild depression, many clinicians start with psychotherapy, exercise, sleep improvement, and nutrition changes first. Medication may be added later if symptoms persist or worsen.
Depression Treatments Without Medication
Not everyone needs—or wants—antidepressants. For mild to moderate depression, non-medication treatments can be very effective, either on their own or alongside medication for more severe cases.
Schedule a confidential consultation with our team below to discuss your symptoms and explore treatment options—whether that’s therapy, lifestyle changes, medication, or a combination—so you can move toward lasting relief with a plan that fits you.
Is Depression a Lifelong Condition? Can Chronic Depression be Resolved?
Depression is a highly heterogeneous disorder with variable outcomes. While it is often described as chronic and recurrent, research consistently shows that not all individuals experience lifelong depression.
According to Monroe et al. (2022), about half of those who experience a major depressive episode will never have a recurrence, while the other half may face repeated episodes throughout their lives.
Chronic or persistent depression—defined as lasting two years or more—affects a minority of patients, with estimates suggesting 20–30% of cases, while the majority recover, sometimes with no further episodes (Richards, 2011; 7).
Can Chronic, Lifelong Depression be Resolved?
The good news is that most people do not remain severely depressed forever. Complete recovery from depression is possible. According to Scott et al. (2023), only about 11–12% of people with chronic conditions experience consistently high depression for years, while the majority eventually improve or experience periods of relief.
Effective treatments—such as cognitive-behavioral therapy and Transcranial magnetic stimulation (TMS)—can reduce symptoms and help people regain functioning, with benefits lasting at least a year (Buhrman et al., 2015). Even in cases of chronic pain or multimorbidity, targeted therapy and medical care improve outcomes (Read et al., 2017; Brandl et al., 2022) (15,13).
Many individuals achieve remission from chronic depression, defined as the absence or near-absence of symptoms and restoration of functioning. However, recovery may not be permanent for everyone, as relapse and recurrence are common, especially in those with early onset, severe symptoms, or comorbid conditions (Comijs et al., 2015; 4; Szymkowicz et al., 2023; 3).
REAL LIFE TESTIMONIAL OF PATIENTS RECOVERING FROM DEPRESSION AND ANXIETY - PSYCHIATRIC SPECIALTY CENTER IN WELLINGTON, FL
Why Depression Feels Like a Constant, Never-ending Battle?
Depression can feel like an unending fight because it affects the mind, body, and relationships all at once. People living with chronic depression often describe it as “depths of emptiness,” “episodic despairing engulfment,” and a “struggle of unending life problems,” which captures the sense of relentless inner conflict (Rhodes et al., 2018). This day-to-day battle is fueled by overlapping biological, psychological, and social factors.
Why Does ONGOING, Persistent Depression Happen?
Chronic or lifelong depression rarely stems from a single cause. Instead, it develops from an interplay of biological, psychological, and social factors that reinforce each other over time.
Biological and Genetic Factors
According to Hölzel et al. (2011), people who develop depression at a younger age, experience longer episodes, or have a family history of mood disorders face a higher risk of chronic depression.
Genetics can increase vulnerability, while biological changes such as dysregulated stress hormones and inflammation may sustain symptoms. For example, Hassamal et al. (2023) found that chronic stress can trigger neuroinflammation—a brain-based immune response—that is linked to more severe, treatment-resistant depression. Other reviews highlight that chronic inflammation, gut microbiome imbalances, and immune system dysfunction all play a role in maintaining depressive symptoms (Pereira et al., 2020; Berk et al., 2013).
Early Life Experiences and Personality
Developmental adversity is another powerful factor. According to Riso et al. (2002), childhood trauma, ongoing stressors, and certain personality traits—such as heightened stress reactivity—significantly increase the likelihood of a persistent depressive course. Chronic pain, disrupted sleep, and medical illnesses can further elevate risk (Ni et al., 2022; Meerlo et al., 2015).
Psychological and Social Contributors
Co-occurring mental health conditions are common. Hölzel et al. (2011) reported that anxiety disorders, personality disorders, and substance abuse frequently overlap with chronic depression.
Social factors also matter. According to Durdurak et al. (2024), loneliness and feeling disconnected—especially in adolescence—strongly predict long-term depressive symptoms. Low social integration and negative social interactions can keep individuals trapped in a cycle of despair (Ambresin et al., 2023; Hussenoeder et al., 2022).
The Stress–Inflammation Loop
Chronic stress doesn’t just affect mood; it reshapes the brain. According to Zheng et al. (2022), repeated stress strengthens maladaptive neural pathways in regions that regulate motivation and mood, making depression more likely to persist. This stress–inflammation loop can make depression more resistant to standard treatments, requiring integrated medical and psychological care.
What Methods are used to Resolve Lifelong (Chronic) Depression? Evidence-Based Approaches
Chronic depression—sometimes called persistent depressive disorder—often requires a multimodal treatment plan.
The most effective strategies combine psychotherapy, medication, and, when needed, advanced brain-stimulation therapies, supported by lifestyle changes.
Psychotherapy
Psychotherapy remains a core treatment for chronic depression. According to Jobst et al. (2016), European psychiatric guidelines recommend psychotherapy with an interpersonal focus as a first-line approach. The Cognitive Behavioral Analysis System of Psychotherapy (CBASP) is designed specifically for chronic depression and has shown superior outcomes compared to standard care (Michalak et al., 2015).
Other evidence-based methods include Cognitive Behavioral Therapy (CBT) and Interpersonal Therapy (IPT), both of which produce moderate to large effects across diverse patient groups (Cuijpers et al., 2023; Hollon et al., 2002). Tailoring therapy to patient preference improves engagement and results (Cohen et al., 2018).
Medication
Antidepressant medications—such as SSRIs, SNRIs, and tricyclics—are widely used.
According to Gabriel et al. (2020), clinical guidelines recommend SSRIs as a first-line treatment, though other agents may be chosen based on side-effect profiles and patient needs.
While medication alone can be effective, about half of patients may not respond to the first drug and may need dose adjustments, switching, or augmentation (Trivedi et al., 2001; Torpey et al., 2008).
Combined Treatment
The strongest evidence supports combining psychotherapy and medication. According to Cuijpers et al. (2020), integrated treatment consistently outperforms either approach alone for chronic depression. This combination is recommended as first-line therapy in most treatment algorithms (Jobst et al., 2016; Rush et al., 1997).
Brain-Stimulation Therapies
For severe or treatment-resistant cases, brain-stimulation options can be life-changing. Electroconvulsive therapy (ECT) remains one of the most effective treatments for refractory depression, though it is usually reserved for cases where other treatments have failed due to potential cognitive side effects (Trivedi et al., 2001).
Non-invasive Transcranial Magnetic Stimulation (TMS) offers an FDA-cleared alternative and shows strong outcomes for patients who do not respond to medication (Marwaha et al., 2022).
Other and Emerging Approaches
Adjunctive strategies can enhance recovery and prevent relapse. According to Xie et al. (2021), regular exercise reduces depressive symptoms and improves overall functioning. New treatments such as esketamine nasal spray and other novel antidepressants are being actively studied for treatment-resistant depression (Stachowicz et al., 2022). Mindfulness-based cognitive therapy (MBCT) also shows promise for improving quality of life and functioning in persistent depression (McPherson et al., 2022).
How to get started resolving your depression?
If you’re struggling with depression, living in Weston, FL, or nearby cities —whether it feels chronic, recurrent, or overwhelming—the most important step is to reach out for professional help.
Psychiatric Specialty Center board-certified therapists, clinicians, and doctors, have decade of experience helping patients relieve depression, anxiety and other mood disorders.
You do not have to face depression alone. Schedule an appointment or a confidential consultation to explore your options and take the first step toward lasting relief. Recovery is possible—and it starts with a conversation. Click the button below to schedule an appointment with Dr. Amanda Darling and get help with your depression today.